The JAMA article I've mentioned in my last two posts provided an interesting sequel. It mentioned lung and bronchus cancers in the group with breast cancer and prostate cancer, those whose incidence has gone up a fair amount, and death rates have gone down.
That confused me as the numbers showed only a smidge more being diagnosed (an 8% increase) and actually a death rate increase in the same ball park (eleven precent). The footnote said a National Lung Screening Trial looking at higher risk individuals concluded low-dose CT screening could reduce death rates by 20%. I had missed this article which was published in the New England Journal of Medicine in 2011 and had over 53,000 subjects who were randomly assigned to screening with either a single chest x-ray or low-dose CT. The point was CT scanning picked up early-stage cancers and their percentage was way up, while the proportion of later-stage cancers actually was less.
Lung cancer is the third most common in both genders in the United States and is the number one cause of cancer-related deaths. If you're a heavy smoker, the chances of your dying from lung cancer go up immensely The CDC webpage on lung cancer risk factors calls cigarette smoking the major issue causing ~90% of all lung cancers in this country.
I've mentioned this before, but let me reiterate my Dad's smoking cessation and mine. He had three rooms in his private practice office and one day realized he had put a lit cigarette in the ashtray of each room, He never smoked again and lived to ninety-four. I smoked as a youngster for four years, never heavily, and I quit as a senior in medical school when I saw one of my VA patients smoking through the trachesotomy he had had for cancer.
The August edition of the Annals of Internal Medicine, published one day after the piece in JAMA, has an article titled "Screening for Lung cancer with Low-Dose Computed Tomography" (AKA a CT scan). This one reviewed four trials of CT screening; only one was large and of good quality. It actually was the research reported in the NEJM article and the project was stopped at six and a half years when it was noted how much lung cancer mortality was reduced.
What's interesting in this new review article is a series of comparisons: you need to screen 320 at-high-risk subjects by low-dose CT scanning to prevent one death from lung cancer and 219 to prevent one death from any cause. That wasn't striking until I read you need to screen 1339 women aged 50 to 59 with mammography to prevent one breast cancer death and 817 people with flexible sigmoidoscopy (a shorter version of the colonoscope that can reach an estimated two of three colon polyps) to prevent one colon cancer death.
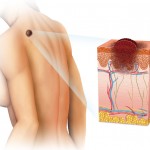
The third category of cancer screening focused on melanoma, the worst of the three common skin cancers (the others are squamous cell and basal cell cancers). In the time frame from 1975 to 2010 the incdence of melanoma went up 199% while the death rate from this tumor went up only 32%. I found a very recent online article on this cancer, reprinted from an April, 2011 publication, by US News and World Report. It focused on its warning signs and prevention as well as treatment.
We live at an altitude of ~5,200 feet, so our exposure to damaging UV rays from sunlight is considerable. My wife drives 55 miles to several times a year to see a dermatologist and the last few years I've gone with her on one of those visits and had a skin check,
Melanomas account for three quarters of all deaths from skin cancer and are felt to result from excessive exposure to UV light. We walk in the early morning and after dark, not during the middle of the day, don't use tanning beds, my wife always wears sunscreen (I confess I don't routinely do so, but I should), and neither of us has "fair or freckled skin' or a family history of this disease.
The NCI says a change in the size or shape, color or texture of an existing mole, one of the black or brown patches that most of us, by adulthood have a number of (10-40 is common).I like the NCI's ABCDE approach to look at moles: A stand for asymmetric, different parts of the skin lesion not looking the same; B means borders that are irregular, shaggy or ill formed (uneven or scalloped); C is for color that varies from part of the mole to another; D is for diameter (melanomas, while they may be smaller, usually are larger than a pencil eraser in size): and E is for evolving (changes in size, shape, color, elevation or even bleeding, crusting/scaling or itching).
Any of these signs should prompt a quick call to your doctor and perhaps a visit to a dermatologist.
Fortunately, the only skin cancer either of us has had thus far was a squamous cell and it was removed by the Mohs technique, in which a section of the lesion is surgically removed by a specially trained physician, and then immediately stained and examined under the microscope to make sure the borders are clear of any tumor. The process is repeated until safe borders are noted.
The last kind of cancer I want to mention is thyroid; during the thirty-five year period its incidence went up 185, but its death rate went down 7%.
In spite of having a first cousin who had this tumor, it was the one I knew the least about. So I went to the MD Anderson Cancer Hospital's website on Thyroid Cancer Prevention and Screening. They mentioned on type that runs in families and is genetically linked, but for most of us, looking at our neck carefully twice a year, having our physician do a cancer-related exam yearly, making sure your salt has iodine, and knowing that most of these lesions occurs in women (3/4s), typically between age 20 and 55 is a good start. One other comment was exposure to radiation, especially in childhood is a significant risk factor.
There are other cancer screening procedures, but those are the common ones. Your physician may have a few more in mind.