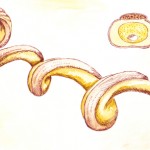
There continues to be considerable controversy over the extent of Lyme Disease in the United States. Its cause is a spirochete, a skinny, long bacteria that is coiled and looks like a microscopic spring. Historically this family of "bugs" was known to have a member that caused syphilis, a scourge of mankind for thousands of years. Then in 1975 a new disease made its first appearance with a cluster of cases in both children and adults in Lyme, Connecticut. Over fifty cases were reported in the first two years of the epidemic, the black-legged tick Ixodes scapularis was found to be the vector that transmits the disease to humans and in 1982 the spirochete Borrelia burgdorferi was identified as the bacteria responsible for the rash, arthritis, cardiac and neurological manifestations of what was eventually termed Lyme disease. The World Health Organization calls the illness Lyme borreliosis and it is widely found in Europe from Turkey to Sweden with nearly 65,000 cases a year, some differences in signs and symptoms and another tick species as the transmitting agent.
Lyme disease has clearly spread from its origin in the northeast US and is now an illness that affects hundreds of thousands yearly. The Center for Disease Control and Prevention (CDC) has a website with extensive information on Lyme Disease, and links to frequently asked questions about the illness. Among those bits of information is the blunt statement that Lyme disease, to a great extent, only occurs in three endemic regions of this country. Those cases occur in the area from northeast Virginia to Maine and some north-central states, including Wisconsin and Minnesota.
But it also can be spread by another tick much further west, especially in California where a different black-legged tick, Ixodes pacificus is the vector. And the CDC's own interactive map of Lyme disease cases from 2001 through 2012 shows it has struck in Florida, Texas and a number of other states, albeit without the number of cases seen in the east and northeast portions of this country.
Humans aren't the only species affected; dogs can get Lyme disease also and the incidence of the illness has markedly increases. A canine vaccine is available. Horses, cattle and cats can also get Lyme, but much less commonly.
A major issue is whether Lyme disease or something quite similar occurs in the South. The debate on that started twenty-five years ago and continues to today.
In 1988, Dr. Edwin Masters, a family practice physician in Missouri and amateur forester, gave a talk on Lyme disease to a forestry association. He had extensively prepared for his lecture and subsequently began to see cases of what he thought was Lyme disease in his own practice. Many had a rash similar to Lyme victims elsewhere (erythema migrans, abbreviated as EM). Some had swollen joints, neurological signs and symptoms and positive blood tests for Lyme disease using the test most commonly available then. Masters reported his cases to the Missouri Department of Health, but found that his reports were ignored.
He didn't give up at that point, but carefully photographed the EM rashes his patients presented with and stored blood samples. In the North the CDC said just having the reach was diagnostic, but denied that was true in the South.
A 1999 paper published by scientists from Amsterdam and New York said that there are ten different species of the spirochete bacteria that is called Borrelia. At that time three were known to cause disease in humans.
A multi-part 2009 blog post in Psychology Today's Emerging Diseases series (written by Pamela Weintraub, the Executive Editor at Discover Magazine) was titled "Rebel with a Cause: The Incredible Dr. Masters." It details the last thirty years of the live of the physician who championed the cause of Southern Lyme disease.
A 2013 Discover Magazine In-Depth report Ticked: The battle over Lyme Disease in the South, tells the story well (I downloaded it for $1.99). In brief, many people who live in the South have had a Lyme-like illness that the Lyme and Tick-Borne Diseases Research Center at Columbia University calls STARI, Southern Tick-Associated Rash Illness. From the CDC's conservative viewpoint this is not Lyme Disease since it has never been clearly proven to be caused by the spirochete Borrelia burgdorferi sense stricto (that translates to "In the strict sense") and, according to the CDC doesn't cause the major complications associated with that illness. Their 2011 webpage on STARI says patents bitten by the Lone Star tick can sometimes develop an EM rash like those of Lyme disease victims, but the skin manifestations of STARI are slightly different and arthritis, cardiac or neurological complications don't occur.
Kerry Clark, a PhD associate professor in the Department of Public Health at the University of South Florida, took up the cudgel for Southern Lyme disease after Masters' death. He is a medical entomologist at USF who had collected and studied ticks for years. After giving a Lyme disease talk in Georgia three years ago, he was approached by a woman from an Atlanta suburb who told him there were many similar cases in her town. Clark collected many ticks from the patchy woodland areas infiltrating the area; most were juvenile (nymph phase) or adult Lone Star ticks.
Several days later he found one engorged tick on his own scalp. Since he has had fatigue, intermittent mental "fuzziness," twitches and a strange recurrent pounding headache.
Clark recently published a major study in the International Journal of Medical Sciences (easily available on the National Library of Medicine website) with the title "Lyme Borreliosis in Human Patients in Florida and Georgia, USA." It gives demographic, clinical and lab data on ten such patients with suspected Lyme disease. Clark and his associates used a newly developed test developed specifically for the genospecies Borrelia burgdorferi. Worldwide this includes more than 20 different "bugs" with seven in North America, but in the past only one had been generally accepted as responsible for Lyme disease. With DNA confirmation, they reported finding other closely-related spirochetes in patients' blood and skin as well as in Lone Star ticks.
My first take was this was an impressive article, but I am aware of those who would treat many patients with a variety of symptoms for "chronic Lyme disease" over extended periods of time using repeated doses of expensive intravenous antibiotics. And there is another subset of physicians, including, unfortunately, one of Clark's co-authors, who use treatment modalities which I view with great skepticism.
If other academic laboratories confirm Clark's work, perhaps we can get to definitive answers and make available tests that help determine when and how to treat patients with atypical Lyme disease.
Having seen diagnoses come and go (e.g., the virus that supposedly caused chronic fatigue syndrome was eventually found to be a lab contaminant), I'm waiting for those confirmatory studies.
babesiosis, caused by the parasite Babesia microti —
a pathogen similar in type and impact to the one that causes
malaria. Ticks in the South also carry other diseases, including
Rocky Mountain Spotted Fever and ehrlichiosis, caused by two
kinds of related bacteria.
The Columbia University Lyme and Tick-borne Disease Research Center's website has a nicely balanced discussion of STARI, Southern Tick-Associated Rash Illness, sometimes called Masters Disease in honor of the now-deceased Missouri family physician who initially reported cases of what was felt to be a Lyme Disease-like illness.
Discover magazine, which I subscribe to, has an In-Depth publication available for $1.99 on the controversy concerning a Lyme disease-like illness in the south. It's well written by Wendy Orent, a PhD anthropologist/science writer who teaches at Emory University; she has also published a controversial book on plague.
Orent was also involved in a debate about the possibility of an H5N1 (bird flu) epidemic. According to Orent, there was no legitimate basis to assume that any large-scale epidemic would ensue as a result of the H5N1 virus.