I recently heard from Kevin Thompson, a Colorado blogger who read one of my posts and wondered if I'd include a link to one of his on my website. I knew of tree nut allergies only in the most general terms, but found his post gripping and, for parents of a child with nut allergies, potentially life-saving.
But I wanted to do some reading on the subject myself and also needed to see what else Kevin had posted on his blog.
Before I move on to his recent ideas on nut allergies, I'd like to mention (and give you a link to) another of Kevin's posts, "10 of the Most Common Food Allergies in Kids." In that one he discusses, in non-technical terms, children's alleges to eggs, milk, soy, wheat, peanuts, tree nuts, fish, shellfish, strawberries and (amazingly) kiwi fruit.
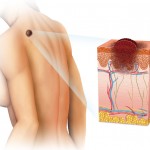
The American Academy of Pediatrics website has a July, 2013 update on diagnosing food allergies in children. That post mentions the most common pediatric food allergies are to dairy products, egg whites, poultry, seafood, wheat, nuts, soy and chocolate. Like any kind of allergy, those to food happen when your immune system, reacting to a substance foreign to your body, produces antibodies, chemicals that usually help to protect you from infections, or as the Mayo Clinic website on allergies says, "unwanted invaders that could make you sick."
The reaction from your immune system leads to inflammation, but the area affected and the seriousness of the reaction varies. What Kevin was talking about is the high end of the spectrum, those forms of allergic responses that can be life-threatening.
Some years back a nurse at the allergy clinic my wife goes to (fifty miles north of us in Cheyenne, Wyoming), asked if someone in the home could give Lynnette her allergy shots. That would mean she didn't have to drive a hundred miles every other week. I was drafted although I had never given shots in my years as a practicing physician. I learned quickly; after all I had performed kidney biopsies and, in my early days in nephrology, stuck large needles into arteries when a patient had acute kidney failure and needed dialysis.
But I needed some onsite drugs in case Lynnette had a medium or, heaven forbid, a major reaction to the allergy shots.
I purchased some over-the-counter Benadryl and our family practice physician wrote us a prescription for epinephrine in the form of an EpiPen (there are other brands). This is an auto-injector, something you slam into the outer thigh of a person having a really serious allergic response to a foreign substance (i.e., an allergen) or to exercise or for unknown reasons. It's available in an adult form with 0.3 milligrams of epinephrine or in a half dose (EpiPen Jr) and I purchased a two-pack that came with a training device.
I hadn't tried that before today, so I just got it out of its box and followed the instructions. I removed the Blue Safety Release, swung the device against my outer thigh and pushed it, hearing a click that, with the actual EpiPen would have meant a needle had extended and, while I held it against my thigh for ten seconds, would have injected me with the (hopefully) life-saving medicine. I would have been comfortable using the actual EpiPen, but thought I should simulate a non-medically-trained person practicing how they would use the real thing.
I hadn't mentioned it yet, but you don't take the time to lower the trousers of the person (whether that's you or someone else) having serious allergic problems to use the EpiPen; it goes right through the cloth in the event of a life-threatening emergency. It does have a needle and it does contain the epinephrine to counteract a major allergic reaction.
The Trainer doesn't contain any medication and has no needle; it's also reusable, so somebody can practice with it until they are comfortable with the procedure.
Why in the world would you do this to yourself or someone else? The website of the American Academy of Allergy Asthma and Immunology describes this condition, medically termed anaphylaxis, as a serious, life-threatening allergic reaction, mostly commonly seen with foods, insect stings, medications and latex exposure. The signs and symptoms typically involve more than one part of the body . They require an immediate injection of epinephrine and a trip to the emergency room (call 911, don't drive the person yourself).
Most commonly, anaphylaxis starts within a few minutes (five to thirty) after exposure to the allergen (the substance to which the person is allergic). It can lead to any combination of: hives, swelling in the throat or elsewhere, wheezing, difficulty swallowing, trouble breathing, a feeling of tightness in the chest, syncope (fainting), vomiting and/or diarrhea with cramps, a feeling of impending doom and/or paleness or redness of the body or face.
Occasionally it can have a delayed start, so I had my wife practice with the EpiPen Trainer also just in case I've left the house after I'd given her the shots, waited fifteen minutes to check the areas where they went in (one on each arm), and recorded the local reaction or lack thereof.
So let's go back to Kevin Thompson's blog post, "How to Keep a Child With Nut Allergies Safe at School."It walks you, as a parent, step by step, through the means to safeguard your child's health after they have been diagnosed with an allergy to nuts (tree nuts or peanuts). I think it's well worth reading if you have a youngster with those kinds of potentially fatal allergic problems. From approaching the school's personnel, to helping the child her- or himself be knowledgable, to ensuring the teachers and others at the school are prepared to deal with an anaphylactic reaction, to considering other options, the post is something I'd recommend you print multiple copies of and pursue with due diligence.
It's best to be prepared and even over-prepared for a life-threatening situation.