My wife and I are supporters of two art museums, one locally and the other in Denver. I also have a personal interest in eye problems, especially cataracts and macular disease, as my father had lost an eye as an intern (a paper cut led to an infection and, in those days, before antibiotics, there was concern about the other eye developing problems, a medical issue called sympathetic ophthalmia). In his late 80s he had a cataract in his remaining eye and, when he was examined by an ophthalmologist at the Cleveland Clinic, was found to have macular degeneration, a chronic eye disease usually seen in people over 50.
I became aware, as I read about Dad's problem, that one day it might become mine as well; one of the risk factors for macular degeneration is a family history of the disease.
I've pasted in a list of symptoms from this condition (copied from a Mayo Clinic website).
- The need for brighter light when reading or doing close work
- Increasing difficulty adapting to low light levels, such as when entering a dimly lit restaurant
- Increasing blurriness of printed words
- A decrease in the intensity or brightness of colors
- Difficulty recognizing faces
- A gradual increase in the haziness of your central or overall vision
- Crooked central vision
- A blurred or blind spot in the center of your field of vision
- Hallucinations of geometric shapes or people, in case of advanced macular degeneration
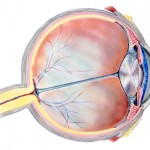
The National Eye Institute, a branch of the NIH, has a fact sheet on age-related macular degeneration (AMD) that's worth looking at if you or someone in your family develops this problem. I'll mention a few things from that website as AMD is a major cause of vision loss in older adults. To begin with the macula is the part of your eyes that gives you the sharpest, most detailed vision. It's the extremely sensitive part of the retina, the layer of tissue at the back of your eye that responds to light, converting images, focused by the eye's lens on this equivalent of camera film, into electrical signals that travel via the optic nerve to the brain. If the macula is damaged, fine points of these images become less clear.
If this happens to a non-artist, someone who doesn't make their living through images they put into a form that others can enjoy, it still leads to less sharp vision. You may have problems reading, driving or recognizing an image such as a face. Since your peripheral vision isn't affected, you'll probably be able to walk around without major difficulty.
But image that you're an artist. You gradually realize your vision is becoming less clear. You used to be able to read an eye chart at the 20/20 level, meaning you can read the same row of small letters on the chart at 20 feet which those with normal vision can. Now your visual acuity, measured when you see your eye specialist, is slipping and you worry that it will affect your ability to paint as well as you once did.
Having 20/20 eyesight does not necessarily mean perfect vision. 20/20 vision only indicates the sharpness or clarity of vision at a distance. There are other important vision skills, including peripheral awareness or side vision, eye coordination, depth perception, focusing ability and color vision that contribute to your overall visual ability.
Some people can see well at a distance, but are unable to bring nearer objects into focus. This condition can be caused by hyperopia (farsightedness) or presbyopia (loss of focusing ability). Others can see items that are close, but cannot see those far away. This condition may be caused by myopia (nearsightedness).
I've written about these medical problems before, but was riveted by a pair of articles I found in two AMA publications yesterday. A Stanford eye surgeon, Dr. Michael F. Marmor, just published a supurb article on Edgar Degas' progressive loss of vision in his later years. Degas was born in Paris in 1834 and died there in 1917. His painting altered from 1860 , when he had essentially normal vision, to 1870 and beyond when first one eye, then the other progressively lost visual acuity. By 1897 he was seeing at a 20/200 level; that means he could would have to be twenty feet away from an eye chart to read the letters that someone with normal vision could read from 200 feet away.
The style and details of his paintings, especially his pastels, have been shown to change as Degas' eye problems progressed, but Dr. Marmor's article calls our attention to one oil painting, Scene from the Steeplechase: The Fallen Jockey. Here's a link to the painting in the National Gallery of Art; it was originally painted in 1866 and reworked by the artist in 1880-81 and again in 1896 with considerable changes made which Dr. Marmor shows can be linked to Degas' declining visual acuity.
A number of other significant artists have demonstrated visual loss in their work. An April, 2007 article in ScienceDaily focuses on Dr. Marmor's work, mentioning he's authored two books on art and eye sight: Degas Through His Own Eyes and The Artists's Eye (I've ordered a copy of the latter book through Amazon).
The Blind with Camera School of Photography website mentions a number of other famous figures from the art world who struggled with visual issues. Among those were El Greco, Rembrandt, Van Gogh, Paul Cezanne, Claude Monet, Mary Cassatt, Camille Pissarro and Auguste Renoir. Georgia O'Keeffe, who lived to the age of 98, also suffered with significant eye disease in her later years; her almost complete loss of eyesight and ill health during the last fifteen years of her life significantly curtailed her artistic productivity. Her eye problems began in 1968, and by 1971 macular degeneration caused her to lose all her central vision.
Monet had cataracts which not only diminished his visual acuity, but also affected his perception of colors. He resisted having surgery, but eventually decided to have one cataract removed. After the operation, according to science writer Carl Zimmer's review of the San Francisco Exploratorium's free publication, Color Uncovered, Monet, like honeybees, was able to see ultraviolet light (normally filtered out by the lens of your eye) and painted water lilies a pale blue. Bees are guided to pollen by light signals we are unable to perceive; Monet had lost a lens to surgery, but gained a spectrum of light perception the rest of us lack.
I have zero talent as a visual artist, but after bilateral cataract surgery my vision is correctable to 20/20...for now.