We were at a fiftieth wedding anniversary party on a weekend night and ate, among other things, baked beans and chocolate cupcakes. So when I saw a dark splotch on a friend's arm I thought he'd spilled something on himself.
He said, "No, I scratched myself this morning on a rusty piece of metal."
"When did you have your last tetanus booster?"
"You know, I don't remember"
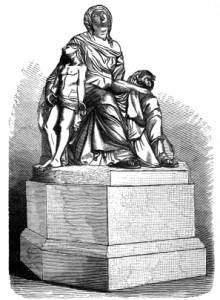
His physician is in solo practice and my friend was unsure of his weekend coverage, so I suggested going to the Urgent Care Clinic our local hospital runs. I nudged him buy showing a 1807 painting of a men with opisothonus, the most extreme muscle spasm one can imagine. At that point he showed me his contact information for his internist and I dialed the number and handed the phone back to him.
As it turned out his doc answers his own messages and told his patient that he had had boosters, but would check his record on the following Monday morning and then call him.
So why was I concerned? After all, the number of cases of tetanus, also called lockjaw, is very small in the United States, usually less than 40 to 60 a year.
That statement holds for most developed countries, but certainly not for the rest of the globe.
Worldwide it's quite a different matter with one source noting over 14,000 cases reported in 2011 and a 5-year death toll of 81,000 reported in 2008.
Still, that's a marked improvement over past years when estimates of a million deaths a year, mostly in Africa and Asia, were the rule. In the late 1980s the World Health Organization (WHO) estimated 787,000 newborns died of neonatal tetanus (NT). That's about 6.7 per every 1,000 live births.
The WHO has an ongoing campaign to eliminate maternal and neonatal (newborn) tetanus and by 2101 the number of NT deaths was estimated at 58,000, still enough souls to fill a mid-sized community, but 93% less than slightly over 20 years previous.
Yes, but a significant number of those who do get it die and having a dirty wound is clearly a risk factor for tetanus.
The tetanus bacteria, an anaerobic (capable of living without oxygen) rod-shaped organism, is found in soil and in the gut flora (the mass of bacteria living in the intestines) of animals and humans. Overall our bowels carry 100 trillion microorganisms, ten times a many as the entire number of cells in a human, with estimates of a hundred times the number of genes as our human genome possesses.
It is not transmitted from person to person, but is present throughout the environment and is commonly found in soil contaminated with manure, and animal and human feces. The incubation period is usually 7 to 8 days, but can range from 3 days to three weeks with shorter incubation timing being associated with heavily contaminated wounds.
Tetanus often begins with muscular stiffness in the jaw, e.g., lockjaw, followed by stiffness in the neck, difficulty swallowing, rigidity of the abdominal muscles, spasms, sweating and fever. Other complications can include vocal cord and/or repsiratory muscle spasm. In especially severe cases long bone or spine fractures can occur as a result of muscle spasms.
The Mayo Clinic's article on tetanus agrees that the tetanus vaccine has made the disease quite rare in developed countries, but notes there are still somewhere about a million cases every year elsewhere in the world (that's quite different from the number I mentioned above, but may represent older figures). There is no cure for this terrible disease and fatality rates, which used to range from 48% upward, are still close to 10% even in settings where modern supportive therapy is available. That may include antibiotics, bed rest in an environment with lights dimmed, noise kept at a minimum and temperature stabilized, drugs for muscle relaxation, sedation and debridement (localized surgery to clean the wound) & possibly tetanus immune globulin.
If no treatment is given, roughly 25% of those infected die and those rates are considerably higher in newborns (typically with umbilical cord infections) and in the elderly without adequate immunization. Yet, until quite recently, most recommendations for tetanus toxoid mention re-immunizing every 10 years until age 65, with no provision for those of us who are older. Below that age, studies of armed forces personnel have shown adequate protection for up to twelve years.
Over the past few years the recommendations for immunization in older adults (age 65 and up) have gradually changed. In late 2010, although there was no formally FDA approved Tdap (Tetanus, diphtheria and pertussis (whooping cough), vaccine for those in that age range, the CDC's Advisory Committee on Immunization Practices (ACIP) suggested Tdap be given to all 65+ adults who were in close contact with infants and others in that older age range could get Tdap. By early 2012 ACIP approved the use of Tdap in all older adults, with one product (Boostrix) being preferred but the use of either of the two kinds of Tdap available in the United States being valid.
Wound management recommendations have similarly changed recently. If more than 5 years have elapsed since the last tetanus booster (which may have been Td), then anyone who is 19 and older should get Tdap.
The last time I got a dirty puncture wound I thoroughly cleaned it and hurried off to the hospital's Urgent Care Clinic, shot record in my hand.
Between tetanus bacilli, flesh-eating strep, drug-resistant staph and all their compatriots I've changed my approach to outdoor work. Although I do much less of it than in years past, I still not infrequently come home with a dirty scratch. I really scrub my hands and occasionally add a topical antibiotic ointment and a band-aid.
I think you should ask your physician when your last tetanus booster was given and see what they'd suggest for supposedly minor cuts and punctures.
You may prevent one or another of the serious bacterial complications most of us have heard about happening, even in our own communities.